Skin cancer
What is it?
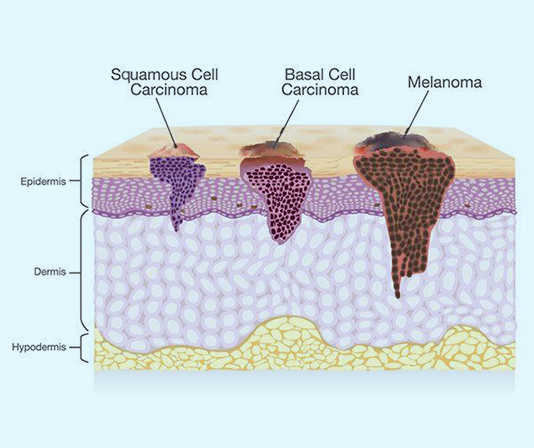
Skin cancer is the abnormal growth of skin cells, most often (but not always) a result of significant exposure to sunlight. As early skin cancer detection allows for a higher chance of successful treatment, it is crucial that you see a doctor as soon as possible if you notice any suspicious changes in your skin. The three major types of skin cancer are basal cell carcinoma, squamous cell carcinoma, and melanoma.

Basal cell carcinoma (BCC) is the most common and most indolent type of skin cancer which starts in the basal cells, the cells which produce new skin cells. BCC often appears as a pearly-like lesion on sun-exposed areas of the skin and very rarely spreads to other areas of the body.
Squamous cell carcinoma (SCC) is the second most common type of skin cancer and are typically locally growing cancers. However, they can be aggressive and spread to other parts of the body if not treated. SCC can appear as scaly red patches, open sores, raised growths, or rough, wart-like skin that may become itchy, crusty, and/or bleed.
黑色素瘤 is less common, but the most serious form of skin cancer as it has a higher chance of spreading to other parts of the body (metastasizing), especially if left untreated. The first indications of melanoma include a visual change in an old mole, or the development of a new pigmented growth.
皮膚癌
What are the symptoms?
What is the cause?
How is it treated?
After surgery management (surgical excision of the cancerous lesion)
What to expect?
- If you experience pain in the biopsy area, you may take over-the-counter Tylenol Extra Strength (Acetaminophen) or Advil/Motrin (Ibuprofen) for pain relief. If you are experiencing severe pain, please contact your physician or go to the emergency room.
How to manage your wound
- After 48 hours, please remove any bandages and wash your incision(s) with soap and water, unless instructed otherwise.
- Please do NOT submerge your incision(s) in water (e.g., swimming, bathing, washing dishes without gloves) until your stitches are removed.
- Keep your incision(s) dry, clean, and exposed to air after 2 days to help the healing process. It is not necessary to cover your incision(s) unless you are exposed to an environment with dirt and dust (e.g., construction zones, workshops).
- If preferred, you may apply a thin layer of Polysporin to the incision site.
- You should have a follow-up appointment booked for 10 to 14 days (5-7 days for lesions on the face) after the surgery. At this appointment, the doctor or nurse will remove any remaining sutures that have not been dissolved and review your pathology report.
- You may have your stitches removed by your family doctor or at a walk-in clinic, however you should still review the pathology report with the doctor who performed the excision.
- Please note that a bit of redness and swelling over the incision is normal. However, watch out for signs of infection such as redness that spreads beyond your incision(s), skin breaking open, and/or pus draining from the incision(s).
- If you experience any of these signs of infection, please call your surgeon to book an appointment as soon as possible or go to the emergency room.
- After your sutures are removed, if your incision is in an area that is exposed to sunlight, it is recommended that you apply sunscreen to the incision site for the entire year following your procedure. This will prevent hyperpigmentation or darkening to the incision site.
- Feeling hardness over the incision site after surgery is normal as it is a result of scar tissue development. After your stitches are removed, you should massage the area 3-4 times a day to help heal the skin and help with the sensitivity that develops with non-use. Over time, the hardness will shrink and soften.